A patient is admitted with anaphylactic shock secondary to a blood transfusion. The patient's spouse asks the nurse to explain how blood can cause a low blood pressure. The nurse responds that with anaphylactic shock the
A. heart muscle weakens and is unable to pump effectively.
B. peripheral blood vessels dilate, and this creates a maldistribution of volume.
C. kidneys excrete large amounts of urine dropping the blood pressure.
D. autonomic nervous system is disrupted dropping blood pressure.
Explanation: Anaphylactic shock is characterized by widespread vasodilation due to the release of histamine and other inflammatory mediators. This vasodilation causes a significant drop in systemic vascular resistance and maldistribution of blood volume, leading to hypotension. The explanation addresses the pathophysiological changes that occur during anaphylactic shock. References: AACN Adult CCRN Certification Review Course, AACN CCRN Exam Handbook.
A patient who is confused and dyspneic is admitted with ABG values that reveal
hypoxemia. Results from insertion of a pulmonary artery catheter are:
PAP 38/18 mm Hg
PAOP10 mm Hg
CI 3.5 L/min/m2
These values are most indicative of
A. hypovolemia.
B. hypervolemia.
C. pulmonary dysfunction.
D. left ventricular failure.
Explanation: The patient’s ABG values show hypoxemia, which is a low level of oxygen in the blood. This can be caused by various pulmonary disorders that impair gas exchange, such as pneumonia, pulmonary edema, pulmonary embolism, or acute respiratory distress syndrome (ARDS). The patient’s PAP (pulmonary artery pressure) is elevated, indicating increased resistance in the pulmonary circulation. This can also result from pulmonary dysfunction, as the lungs become stiff and inflamed, or from pulmonary hypertension, which is a chronic condition that affects the small arteries in the lungs. The patient’s PAOP (pulmonary artery occlusion pressure) is normal, suggesting that the left ventricle is not failing and that the patient is not hypovolemic or hypervolemic. The patient’s CI (cardiac index) is also normal, indicating adequate cardiac output. Therefore, the most likely cause of the patient’s hypoxemia and dyspnea is pulmonary dysfunction.
A patient is admitted with Gl bleeding. During the assessment, the nurse notes the patient to be tremulous, anxious, and startles every time he is touched by the nurse. Which of the following is the most pertinent part of the patient's history to obtain?
A. last alcohol intake
B. medication history
C. time of last meal
D. psychiatric history
Explanation:
The patient’s symptoms of tremulousness, anxiety, and startle response suggest that he
may be experiencing alcohol withdrawal, which can occur within hours to days after the last
drink. Alcohol withdrawal can cause severe complications, such as seizures, delirium
tremens, and death, if not treated promptly and appropriately. Alcohol withdrawal can also
worsen GI bleeding by increasing gastric acid secretion, impairing clotting factors, and
causing hypertension and tachycardia. Therefore, the most pertinent part of the patient’s
history to obtain is the last alcohol intake, which can help determine the risk and severity of withdrawal and guide the management of the patient.
References:
Management of moderate and severe alcohol withdrawal syndromes: This article
states that “Symptoms of alcohol withdrawal occur because alcohol is a central
nervous system depressant. When a person drinks frequently, the brain
compensates for alcohol’s depressant effects by increasing the activity of
excitatory neurotransmitters, such as norepinephrine, serotonin, dopamine, and
glutamate, and reducing the activity of inhibitory neurotransmitters, such as
gamma-aminobutyric acid (GABA). When alcohol intake is abruptly discontinued or
reduced, this neuroadaptation is unmasked, resulting in a hyperexcitable state that
is responsible for the characteristic withdrawal symptoms.”
Alcoholic Gastritis: Causes, Symptoms and Treatment: This article states that
“Alcohol Gastritis is a type of acute gastritis and is caused by excessive alcohol
consumption. The sudden inflammation of the stomach lining can be very painful
and cause severe stomach cramping, irritability and vomiting. While consuming too
much alcohol is the main cause of Alcohol Gastritis, it often develops in connection
with some sort of infection, direct irritation or localized tissue damage. It can be
caused by: Taking non-steroidal, anti-inflammatory medications like aspirin or
ibuprofen (i.e., NSAIDs). Certain bacterial infections. Bile reflux from proximal
small intestine. Autoimmune disorders.”
Can You Get Internal Bleeding from Alcohol Abuse: This article states that “Over
time, alcohol abuse starts to eat away at the stomach lining. Continued drinking
sets the stage for alcoholic gastritis to develop. Under these conditions, internal
bleeding from alcohol abuse takes the form of blood oozing from stomach lines on
an ongoing basis.”
A patient who sustained acute head trauma exhibited intermittent unconsciousness prior to admission. The patient is disoriented initially and exhibits rapid deterioration in neurological status shortly after admission. X-rays reveal a right temporal bone fracture, and a diagnosis of epidural hematoma is made. The deterioration in the patient's condition is most likely associated with
A. arterial bleeding.
B. venous bleeding.
C. clot formation.
D. intracranial aneurysm.
Explanation:

An epidural hematoma is a collection of blood that forms between the skull and the dura
mater, the outermost layer of the meninges that cover the brain. The most common cause
of an epidural hematoma is a head injury that fractures the temporal bone and tears the
middle meningeal artery, which runs along the inner surface of the skull. Arterial bleeding is
under high pressure and can rapidly expand the hematoma, compressing the brain and
causing neurological deterioration. A typical symptom of an epidural hematoma is a brief
loss of consciousness followed by a lucid interval and then a rapid decline in
consciousness and brain function. This condition requires urgent surgical evacuation of the
hematoma to prevent brain damage or death12. Venous bleeding, clot formation, and
intracranial aneurysm are not the main factors associated with the deterioration of the
patient’s condition in this case.
Which of the following signs is most frequently associated with meningitis?
A. positive Trousseau's
B. positive Cullen's
C. positive Kernig's
D. positive Babinski's
Explanation:
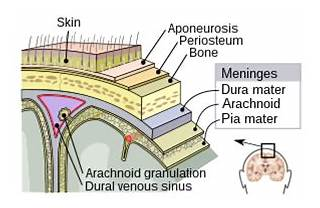
A positive Kernig’s sign is a clinical test for meningitis that involves flexing the hip and knee
of the patient and then extending the knee. If the patient feels pain or resistance in the
lower back or hamstring, the test is positive. A positive Kernig’s sign indicates irritation of
the meninges, the membranes that cover the brain and spinal cord. A positive Trousseau’s
sign is a sign of hypocalcemia that involves carpal spasm after inflating a blood pressure
cuff. A positive Cullen’s sign is a sign of retroperitoneal bleeding that involves bruising
around the umbilicus. A positive Babinski’s sign is a sign of upper motor neuron lesion that
involves fanning of the toes when the sole of the foot is stroked.
The water retention associated with SIADH is characterized by
A. fluid intake greater than UO, weight gain, and increased urine osmolality and sodium.
B. UO greater than fluid intake, extreme weight gain, and mild (2+) pitting edema.
C. UO greater than fluid intake and severe (4+) pitting edema.
D. fluid intake greater than UO, increased serum osmolality and sodium, and severe (4+) pitting edema.
Explanation:
The syndrome of inappropriate antidiuretic hormone (SIADH) is characterized by excessive
release of antidiuretic hormone (ADH), leading to water retention. This results in fluid intake
being greater than urine output (UO), weight gain due to fluid retention, and concentrated
urine with increased osmolality and sodium levels. SIADH does not typically present with
severe pitting edema or increased serum osmolality and sodium.
References: =
CCRN (Adult) Certification Review Course Online: Endocrine Emergencies.
American Association of Critical-Care Nurses (AACN). (2024). CCRN Exam
Handbook. Retrieved from AACN CCRN Exam Handbook
Adult CCRN/CCRN-E/CCRN-K Certification Review Course Online. AACN
The family of a patient requests permission to administer traditional herbs to the patient. Which of the following should be the nurse's first action?
A. Inform the family that herbal therapy is not appropriate in the hospital.
B. Consult with the pharmacist on the effects of the specific herbs.
C. Allow the patient to take the herbs because they are natural.
D. Obtain an order for the herbs.
Explanation: Verified Answer: B. Consult with the pharmacist on the effects of the specific
herbs. Herbal therapy is a type of complementary and alternative medicine (CAM) that
uses plants or plant extracts to treat various health conditions. Many patients use herbal
therapy for various reasons, such as cultural beliefs, personal preferences, or
dissatisfaction with conventional medicine. However, herbal therapy is not without risks and
challenges, especially in the hospital setting. Some of the potential problems include lack of
standardization, quality control, and regulation of herbal products; adverse effects and
interactions with other medications; and ethical and legal issues regarding informed
consent, documentation, and liability12. Therefore, the nurse’s first action should be to
consult with the pharmacist on the effects of the specific herbs that the family wants to
administer to the patient. The pharmacist can provide information on the safety, efficacy, dosage, and compatibility of the herbs with the patient’s condition and current medications.
The nurse should also inform the patient’s primary provider and obtain an order for the
herbs before allowing the patient to take them. The nurse should document the use of
herbal therapy in the patient’s medical record and monitor the patient for any adverse
effects or changes in response to other treatments. Informing the family that herbal therapy
is not appropriate in the hospital is not respectful of the patient’s autonomy and cultural
values. Allowing the patient to take the herbs without consulting the pharmacist and
obtaining an order is not safe and may violate the hospital’s policies and standards of care.
The primary pathophysiology underlying acute respiratory failure in a patient with head trauma involves
A. hypercapnia related to decreased minute ventilation.
B. shifting of oxyhemoglobin dissociation curve to the left.
C. increased arterial oxygenation related to increased intrapulmonary shunt.
D. dehydration related to diabetes insipidus.
Explanation: In a patient with head trauma, the primary pathophysiology underlying acute
respiratory failure often involves hypercapnia due to decreased minute ventilation. Head
trauma can impair the central nervous system's ability to regulate breathing, leading to
inadequate ventilation and a build-up of carbon dioxide (CO2) in the blood. Other factors
like shifting of the oxyhemoglobin dissociation curve, increased intrapulmonary shunt, and
dehydration due to diabetes insipidus may be present but are not the primary causes.
References: CCRN Exam Handbook, AACN, page 25, section on Respiratory.
A patient with a history of asthma presents with acute onset of dyspnea, a non-productive cough, and tachypnea. He is very anxious, restless, and tachycardic. Which of the following is a first-line drug for these symptoms?
A. leukotriene inhibitor
B. anticholinergic
C. mast cell stabilizer
D. beta-agonist
Explanation: Beta-agonists are the first-line drugs for acute asthma exacerbations
because they rapidly reverse bronchoconstriction and improve airflow. They act by
stimulating beta-2 receptors in the smooth muscle of the airways, causing relaxation and
dilation. Beta-agonists can be administered by inhalation, nebulization, or injection.
Examples of beta-agonists include albuterol, levalbuterol, and terbutaline.
References:
Management of Acute Asthma Exacerbations | AAFP: This article states that
“Quick-relief medicines include: Albuterol (ProAir HFA, Proventil-HFA, Ventolin
HFA, others). Levalbuterol (Xopenex, Xopenex HFA).”
Asthma attack - Diagnosis and treatment - Mayo Clinic: This article states that “If
you’re in the yellow zone, the plan will tell you how many puffs of your quick-relief
medicine to take and how often you can repeat the dose. Young children or people
who have difficulty with an inhaler use a device called a nebulizer to inhale the
medicine in a mist. Quick-relief medicines include: Albuterol (ProAir HFA,
Proventil-HFA, Ventolin HFA, others). Levalbuterol (Xopenex, Xopenex HFA).”
A patient is intubated, is unable to follow simple commands, and has no history of alcohol abuse. The patient has become increasingly disoriented and confused over the past 24 hours. After assessment and treatment of pain, the best medication intervention for management is
A. lorazepam (Ativan).
B. cisatracurium (Nimbex).
C. midazolam (Versed).
D. dexmedetomidine (Precedex).
Explanation: Dexmedetomidine (Precedex) is the most appropriate medication for managing agitation and delirium in a critically ill intubated patient. It provides sedation without significant respiratory depression and has analgesic properties, which makes it suitable for patients who are disoriented and confused. Unlike benzodiazepines (lorazepam and midazolam) or neuromuscular blockers (cisatracurium), dexmedetomidine can improve delirium outcomes and facilitates easier weaning from mechanical ventilation. References: = AACN Certification and Core Review for High Acuity and Critical Care, 7th Edition, AACN Handbook for CCRN Certification, pp. 57-60.
A unit council is requesting to change a documentation screen of the electronic health record (EHR) at a large health system. The change was not discussed with the department prior to the request and was denied by the EHR committee. Which of the following strategies will most likely lead to accomplishing the team's goals?
A. Have nursing leadership evaluate the proposal before resubmitting the request.
B. Discuss the proposed solution with stakeholders to determine buy in.
C. Work with key staff members to rewrite the request to present at the next meeting.
D. Attempt to change the process through another format.
Explanation: When seeking to make changes to a documentation screen in the electronic health record (EHR), it is crucial to involve all relevant stakeholders to ensure their buy-in and support. This includes discussing the proposed changes with those who will be directly impacted by it and obtaining their feedback. This collaborative approach can help in identifying potential issues and garnering the necessary support for the proposal, increasing the likelihood of it being accepted by the EHR committee in the future.References: = CCRN Exam Handbook, page 58
Which of the following should the nurse expect in a patient with papillary muscle dysfunction?
A. mitral insufficiency
B. aortic stenosis
C. mitral stenosis
D. aortic insufficiency
Explanation: Papillary muscle dysfunction, often resulting from myocardial infarction, can lead to mitral insufficiency (mitral regurgitation). The papillary muscles support the mitral valve, and if they are damaged, the valve may not close properly, causing blood to flow backward into the left atrium during systole. This condition is not associated with aortic stenosis, mitral stenosis, or aortic insufficiency. References: = CCRN Exam Handbook, AACN Adult CCRN Certification Review Course
| Page 5 out of 13 Pages |
| Previous |