In a patient with hypertensive crisis, neurologic changes are caused by
A. excessive secretion of catecholamines.
B. vasospasm of the cerebral arterioles.
C. hypoxemia as a result of pulmonary interstitial edema.
D. increased ICP as a result of loss of cerebral autoregulation.
Explanation: In hypertensive crisis, neurologic changes are often caused by increased intracranial pressure (ICP) as a result of loss of cerebral autoregulation. Autoregulation normally maintains consistent cerebral blood flow despite changes in systemic blood pressure. In hypertensive crisis, the extremely high blood pressure overwhelms these mechanisms, leading to increased cerebral blood flow, disruption of the blood-brain barrier, and cerebral edema, which subsequently increases ICP and causes neurologic changes.References: = CCRN Exam Handbook, page 48
A patient with end-stage COPD who has failed multiple mechanical ventilation weaning trials communicates a desire to discontinue mechanical ventilation and be extubated. Which of the following is a nurse's best response?
A. Advocate with the care team for a withdrawal of treatment plan.
B. Encourage the patient to continue with current medications and attempts to wean.
C. Explore the patient's reasons for the request and understanding of potential consequences.
D. Refer the patient's request to the healthcare facility's ethics committee for review.
Explanation: The nurse’s best response is to explore the patient’s reasons for the request and understanding of potential consequences, as this demonstrates respect for the patient’s autonomy and dignity, as well as provides an opportunity to assess the patient’s decision-making capacity, goals of care, and preferences for end-of-life care. The nurse should also provide emotional support, education, and symptom management to the patient and family. Advocating with the care team for a withdrawal of treatment plan, encouraging the patient to continue with current medications and attempts to wean, or referring the patient’s request to the healthcare facility’s ethics committee for review are not appropriate responses, as they may undermine the patient’s right to self-determination, impose the nurse’s own values or beliefs, or delay the implementation of the patient’s wishes.
A patient who underwent bowel resection surgery due to small bowel rupture is tachycardic and hypotensive. A nurse calls the on-call surgical resident and reports the findings. No new orders are received. The nurse should continue to monitor the patient and
A. notify the charge nurse during nightly rounds.
B. inform the clinical manager in the morning.
C. initiate the rapid response team.
D. consult the nearest nursing colleague.
Explanation: The patient's tachycardia and hypotension following bowel resection surgery indicate potential severe complications such as hemorrhage or septic shock, which require immediate intervention. If the on-call surgical resident does not provide new orders, the nurse must act promptly to prevent further deterioration by initiating the rapid response team (RRT). The RRT can provide critical interventions and facilitate timely transfer to a higher level of care if needed. References: = CCRN Exam Handbook, AACN Adult CCRN Certification Review Course
A patient admits to a nurse that he has struggled with depression and feelings of isolation
and abandonment since moving into a nursing home last year,
but he has recently started taking an anti-depressant. The patient states, "Sometimes it
takes everything I've got just to go on each day." Which of the
following is the nurse's best initial response?
A. "You sound like you've been really unhappy. Have you thought about harming yourself?"
B. "Those feelings should resolve when the medication you've started has a chance to take effect."
C. "I understand how you feel. We all get that way when we're depressed."
D. "Have you talked to anyone about what is bothering you?"
Explanation: This is the nurse’s best initial response, as it expresses empathy, validates
the patient’s feelings, and assesses the patient’s risk of suicide. Depression is a common
and serious mental health condition that affects older adults, especially those living in nursing homes. Depression can cause persistent sadness, hopelessness, loss of interest,
and suicidal thoughts or behaviors. The nurse should screen the patient for depression
using a validated tool, such as the Patient Health Questionnaire (PHQ-9) 1, and ask about
any suicidal ideation or plans. The nurse should also provide emotional support, education,
and referral to appropriate resources for the patient.
B. “Those feelings should resolve when the medication you’ve started has a chance to take
effect.”
This is not the nurse’s best initial response, as it dismisses the patient’s feelings, implies
that the patient just needs to wait for the medication to work, and does not address the
patient’s psychosocial needs. Antidepressants are one of the treatment options for
depression, but they may take several weeks to show their full effect, and they may not
work for everyone. The nurse should also explore other factors that may contribute to the
patient’s depression, such as social isolation, loss of autonomy, chronic illness, or grief,
and offer interventions that may help the patient cope, such as counseling, psychotherapy,
cognitive-behavioral therapy, or social activities.
C. “I understand how you feel. We all get that way when we’re depressed.”
This is not the nurse’s best initial response, as it assumes that the nurse knows how the
patient feels, minimizes the patient’s experience, and generalizes the patient’s condition.
Depression is not a normal or inevitable part of aging, and it affects each person differently.
The nurse should not compare the patient’s feelings to their own or to others, but rather
acknowledge and respect the patient’s unique perspective and situation. The nurse should
also avoid using words like “we” or “you” that may create a sense of distance or judgment,
and instead use words like “I” or “me” that may convey a sense of empathy or rapport.
D. “Have you talked to anyone about what is bothering you?”
This is not the nurse’s best initial response, as it may sound like the nurse is trying to avoid
listening to the patient, or that the patient is bothering the nurse with their problems. The
nurse should not imply that the patient should talk to someone else, but rather show
interest and willingness to listen to the patient. The nurse should also use open-ended
questions that invite the patient to share more, such as “How are you feeling today?” or
“What has been on your mind lately?” The nurse should also use active listening skills,
such as nodding, paraphrasing, reflecting, or summarizing, to demonstrate understanding
and engagement.
Which of the following suggests acute peripheral arterial insufficiency?
A. positive Homans' sign
B. capillary refill time less than 2 sec
C. weak equal bilateral pedal pulses
D. sudden, severe pain at rest
Explanation: Acute peripheral arterial insufficiency typically presents with sudden, severe pain at rest, which may be accompanied by other signs such as pallor, paresthesia, paralysis, pulselessness, and poikilothermia (the six P's). This condition indicates a critical reduction in blood flow to the affected extremity, requiring immediate medical attention. References: AACN Adult CCRN Certification Review Course, AACN CCRN Exam Handbook.
A 22-year-old trauma patient sustained multiple fractures after a fall. The patient fell 50 feet from a cliff while rock climbing without a harness. The patient is intubated and sedated with casts to bilateral lower extremities. The nurse should recognize that young adults are
A. more likely to engage in risk-taking behaviors.
B. developmentally vulnerable to peer pressure in extreme sports.
C. working through trust issues that cause them to test limits.
D. influenced by long-time intervals spent in virtual reality.
A nurse is performing medication reconciliation during a patient's admission. To determine the patient's current understanding of the medication furosemide (Lasix), which of the following is the best statement by the nurse?
A. "Can you explain to me what furosemide (Lasix) does for you?"
B. "Do you take the furosemide (Lasix) for your hypertension?"
C. "Which of your medications help to remove extra fluid?"
D. "When is the best time of day to take furosemide (Lasix)?"
Explanation: Asking the patient to explain what furosemide (Lasix) does for them assesses their understanding and allows the nurse to gauge their knowledge and correct any misconceptions. This method is more effective than asking yes/no questions, as it provides a comprehensive insight into the patient's medication literacy. References: = AACN Handbook for CCRN Certification, pp. 102-105.
After the administration of haloperidol (Haldol), a nurse should monitor closely for
A. prolonged QT interval and cardiac dysrhythmias.
B. respiratory failure and cardiac failure.
C. widened QRS complex.
D. increased agitation.
Explanation:
Haloperidol has a known side effect of prolonging the QT interval, which can lead to
cardiac dysrhythmias123. Therefore, after the administration of haloperidol, it is important
for a nurse to monitor for a prolonged QT interval and cardiac dysrhythmias123. This is
why continuous cardiac monitoring is recommended if repeated doses are given1.
A patient is 2 days post MI. The patient was stable until this morning, when severe chest discomfort developed. Assessment reveals:
BP70/palpable
HR122
RR38
PAOP28 mm Hg, with large V waves
CI1.6 L/min/m2
Cool, clammy skin
Inspiratory crackles throughout the lung field
Loud blowing holosystolic murmur at the apex
The patient's present clinical status is most likely a result of
A. papillary muscle rupture.
B. cardiac tamponade.
C. acute aortic insufficiency.
D. ventricular septal defect
Explanation: The patient’s present clinical status is most likely a result of a ventricular septal defect (VSD), which is a hole in the wall between the left and right ventricles. A VSD can occur as a mechanical complication of MI, usually within the first week, due to necrosis and rupture of the ventricular septum. A VSD causes a left-to-right shunt of blood, which leads to increased pulmonary pressure, pulmonary edema, and reduced cardiac output. The patient’s symptoms and signs are consistent with a VSD, such as severe chest pain, hypotension, tachycardia, respiratory distress, high PAOP with large V waves, low CI, cool and clammy skin, inspiratory crackles, and a loud blowing holosystolic murmur at the apex. A papillary muscle rupture, a cardiac tamponade, and an acute aortic insufficiency are other possible mechanical complications of MI, but they have different clinical manifestations. A papillary muscle rupture causes acute mitral regurgitation, which presents with a soft systolic murmur at the apex and pulmonary congestion1. A cardiac tamponade causes compression of the heart by pericardial fluid, which presents with hypotension, muffled heart sounds, and jugular venous distension2. An acute aortic insufficiency causes backflow of blood from the aorta to the left ventricle, which presents with a diastolic decrescendo murmur at the left sternal border and a wide pulse pressure3.
Which of the following intubated patients is most at risk for developing ventilator-associated pneumonia (VAP)?
A. 68-year-old patient, 142 kg, from an assisted living facility with COPD and dialysisdependent renal disease
B. 84-year-old patient, 38 kg, from a skilled nursing facility receiving chemotherapy for colorectal cancer
C. 91-year-old patient, 54 kg, from home with osteoporosis and hypothyroidism
D. 72-year-old patient, 81 kg, from a nursing home with heart failure and chronic bronchitis
Explanation: Among the options, the 68-year-old patient with COPD and dialysisdependent
renal disease is at the highest risk for developing VAP. This is due to multiple
risk factors including advanced age, chronic obstructive pulmonary disease (COPD), which
predisposes to poor lung function and clearance of secretions, and the
immunocompromised state from dialysis-dependent renal disease. The patient's higher
body weight can also contribute to complications in mobility and ventilation management,
further increasing the risk of VAP.
References: =
CCRN (Adult) Certification Review Course Online: Infectious Disease and
Pulmonary Infections.
American Association of Critical-Care Nurses (AACN). (2024). CCRN Exam
Handbook. Retrieved from AACN CCRN Exam Handbook
Adult CCRN/CCRN-E/CCRN-K Certification Review Course Online. AACN
When caring for a patient with septic shock secondary to osteomyelitis, which of the following laboratory tests will best monitor response to therapy?
A. basic metabolic panel
B. complete blood count
C. erythrocyte sedimentation rate
D. blood cultures
Explanation: Blood cultures are the most definitive method to diagnose sepsis and monitor the response to therapy2. They can identify the causative organism and help guide antibiotic therapy2. In the case of osteomyelitis leading to septic shock, blood cultures can help confirm the presence of an ongoing systemic infection1. Other tests like the basic metabolic panel, complete blood count, and erythrocyte sedimentation rate can provide supportive information, but they are not as specific or definitive for monitoring response to therapy in septic shock secondary to osteomyelitis123.
A patient with a C5 spinal cord injury calls the nurse every 15 minutes with requests for juice, water, and repositioning. Which of the following is the nurse's best response?
A. "You need to be repositioned only every 2 hours."
B. "You are safe. Nothing will happen to you."
C. "I will check on you every 30 minutes."
D. "I will get someone to sit with you."
Explanation:
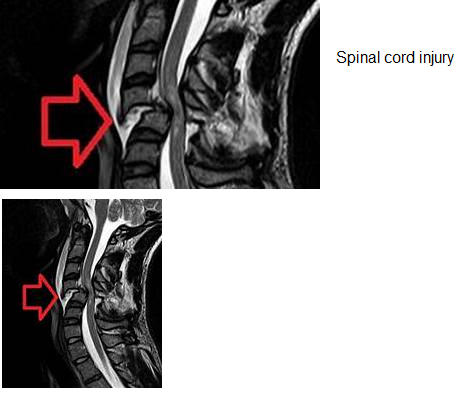
The patient with a C5 spinal cord injury may have anxiety, fear, or depression due to the
loss of function and independence. The patient may also have difficulty breathing,
swallowing, or regulating body temperature. The patient may call the nurse frequently to
seek reassurance, attention, or comfort. The nurse should respond with empathy and
compassion, and provide the patient with emotional support and psychological counseling.
The nurse should also assess the patient’s physical needs and provide adequate hydration,
nutrition, and skin care. The nurse should not dismiss the patient’s requests, ignore the
patient’s feelings, or limit the patient’s contact with the nurse. The nurse should also not
give false reassurance or minimize the patient’s concerns. Therefore, the best response is
to get someone to sit with the patient, such as a family member, a friend, or a volunteer.
This will help the patient feel less isolated, anxious, or depressed, and provide the patient
with a sense of security and companionship.
| Page 4 out of 13 Pages |
| Previous |