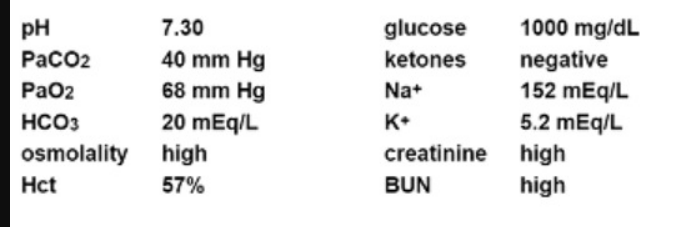
An unconscious patient presents with the following laboratory values:
Appropriate management of this patient should include
A. IV hydration.
B. hemodialysis.
C. intubation.
D. osmotic diuresis.
Explanation: The laboratory values indicate hyperosmolar hyperglycemic state (HHS), characterized by high glucose levels, high osmolality, and dehydration. The primary management includes aggressive IV hydration to correct dehydration and improve circulation. Hemodialysis and intubation are not immediate priorities unless there are other indications, and osmotic diuresis is not appropriate in this context. References: = CCRN Exam Handbook and AACN's Certification Review Course materials.
The most appropriate therapy for carboxyhemoglobinemia is
A. 100% O2 administration.
B. inhaled corticosteroids
C. hyperventilation.
D. aerosolized beta-agonists.
Explanation: The most appropriate therapy for carboxyhemoglobinemia, which is carbon monoxide poisoning, is the administration of 100% oxygen. This treatment helps to displace carbon monoxide from hemoglobin, allowing oxygen to bind to hemoglobin and be transported to tissues more effectively. High-flow oxygen can significantly reduce the halflife of carboxyhemoglobin, facilitating faster recovery.References: = CCRN Exam Handbook, page 30
Which of the following are physiologic effects of pulmonary contusion?
A. increased dead space and decreased airway resistance
B. increased gas diffusion and decreased lung compliance
C. increased airway resistance and decreased gas diffusion
D. increased lung compliance and decreased dead space
Explanation: Pulmonary contusion leads to damage to lung parenchyma, resulting in alveolar hemorrhage and edema. This causes increased airway resistance and decreased gas diffusion due to the inflammatory response and accumulation of fluid within the alveoli, impairing effective gas exchange and reducing lung compliance.References: = CCRN Exam Handbook, page 40
A patient is experiencing lower left quadrant pain with guarding, as well as abdominal
distention and rigidity. KUB reveals free air in the abdominal
cavity. Vital signs are:
BP76/40
HR130
RR32
T101.7° F (38.7°C)
A nurse would suspect
A. perforated bowel.
B. paralytic ileus.
C. appendicitis.
D. acute pancreatitis.
Explanation: The clinical presentation of lower left quadrant pain with guarding, abdominal distention, rigidity, and free air in the abdominal cavity on a KUB (kidney, ureter, and bladder) radiograph strongly suggests a perforated bowel. The presence of free air indicates that there is a breach in the gastrointestinal tract, allowing air to escape into the peritoneal cavity. The patient's vital signs, including hypotension (BP 76/40), tachycardia (HR 130), tachypnea (RR 32), and fever (T 101.7°F), are consistent with sepsis and shock, which are common complications of bowel perforation. References: CCRN Exam Handbook, AACN, page 30, section on Gastrointestinal.
A nurse admits a patient awaiting surgery for an unstable pelvic fracture following a fall in which no other injuries were sustained. The nurse should prioritize
A. transportation to radiology for an MRI.
B. type and crossmatch PRBC prior to surgery.
C. placement of a binder across the patient's hips.
D. administration of a sedative to reduce movement.
Explanation: In the context of an unstable pelvic fracture, placing a binder across the patient's hips is crucial to stabilize the fracture and reduce the risk of further internal bleeding and damage. This intervention helps in temporarily stabilizing the pelvis until definitive surgical treatment can be performed. Transporting the patient for an MRI is not the immediate priority, as the primary goal is to stabilize the patient. Type and crossmatching PRBCs are important but should follow immediate stabilization measures. Administering a sedative to reduce movement can be considered, but it is not the top priority over physical stabilization of the fracture. References: = CCRN Exam Handbook, AACN Adult CCRN Certification Review Course
An older adult patient has been in the unit for 60 hours. The patient has received benzodiazepines for agitation, opioids for persistent pain, and bronchodilators. The patient reports that there is too much noise, and they cannot get peace and quiet. The nurse should evaluate for
A. sleep disturbances.
B. an anxiety disorder.
C. situational depression.
D. acute manic episodes.
Explanation: The patient who has been in the unit for 60 hours and reports agitation, noise disturbances, and an inability to get peace and quiet may be experiencing sleep disturbances. Factors such as the ICU environment, frequent interventions, and the medications being administered (e.g., benzodiazepines, opioids, and bronchodilators) can significantly disrupt sleep patterns, leading to further agitation and delirium. Addressing the patient's sleep hygiene and implementing measures to promote rest can be beneficial. References: = CCRN Exam Handbook, page 52
During the monthly code team review, it is noted that regulators have been consistently missing from the O2 tanks. Which of the following is a nurse's best action?
A. Document on the daily flow sheets when the regulators are missing.
B. Inform the nurse manager of the need for more regulators.
C. Form a task force to try to find a solution.
D. Report the missing regulators to the shift supervisor.
Explanation: The absence of regulators from O2 tanks is a serious issue that can affect patient care1. The nurse manager is in a position to address this problem effectively by ensuring the availability of necessary equipment2. Therefore, the best action would be to inform the nurse manager of the need for more regulators123. While documenting the issue and reporting to the shift supervisor are important, they do not directly address the problem. Forming a task force could be helpful, but it might take more time to implement solutions23.
A patient underwent bariatric surgery for weight loss 3 days ago. The patient appears
anxious, restless, and reports increased abdominal pain over the last 24 hours. The nurse
palpates mild subcutaneous crepitus over the neck. Vital signs are:
BP 106/64
HR 128
RR 27
T 100.4° F (38°C)
Which action should the nurse anticipate?
A. Obtain labs.
B. Administer a 1000 mL bolus of normal saline.
C. Provide broad spectrum antibiotics.
D. Prepare the patient for surgery.
Explanation: The signs and symptoms described in the patient post-bariatric surgery, including anxiety, restlessness, increased abdominal pain, and subcutaneous crepitus over the neck, suggest a potential anastomotic leak, which is a surgical emergency. Given the vital signs indicating possible sepsis or shock (elevated heart rate, increased respiratory rate, and fever), immediate surgical intervention is likely required to repair the leak and prevent further complications. References: CCRN Exam Handbook, AACN, page 30, section on GI surgical emergencies.
The spouse of a critically ill patient is indecisive, withdrawn, and tells the nurse, "I feel so helpless." Appropriate nursing interventions include
A. offering solutions to problems identified by the spouse.
B. encouraging other family members to make necessary decisions.
C. providing reassurance that visiting is not always necessary.
D. identifying and reinforcing the spouse's support systems.
Explanation: When dealing with a spouse who feels helpless, the most effective nursing intervention is to identify and reinforce their support systems. This helps the spouse feel less isolated and more empowered. Offering solutions to problems, encouraging other family members to make decisions, or providing reassurance that visiting is not necessary do not directly address the spouse's feelings of helplessness and may even contribute to feelings of exclusion or inadequacy. References: = CCRN Exam Handbook, AACN Adult CCRN Certification Review Course
A patient who experienced a blunt chest trauma in an automobile crash is admitted with multiple rib fractures. The patient is dyspneic and hypotensive and is reporting left shoulder pain. On auscultation, a nurse notes that bowel sounds can be heard over the lower left thorax. These findings are consistent with
A. ruptured abdominal viscus.
B. ruptured diaphragm.
C. flail chest.
D. mediastinal shift.
Explanation: The patient’s findings are consistent with a ruptured diaphragm, which is a tear in the muscle that separates the chest and abdominal cavities. A blunt chest trauma can cause a sudden increase in intra-abdominal pressure, which can rupture the diaphragm and allow abdominal organs to herniate into the thorax. This can cause dyspnea, hypotension, shoulder pain, and bowel sounds over the lower thorax. A ruptured abdominal viscus would cause peritonitis, which would present with abdominal pain, distension, fever, and signs of sepsis. A flail chest would cause paradoxical chest movement, respiratory distress, and cyanosis. A mediastinal shift would cause tracheal deviation, decreased breath sounds, and jugular venous distension.
The purpose of administering a sodium nitroprusside (Nipride) drip after a carotid endarterectomy is to
A. promote myocardial contractility and thus enhance cerebral perfusion.
B. increase coronary perfusion and thus increase cardiac output
C. decrease MAP and thus prevent hemorrhage at the operative site.
D. increase afterload and thus promote vessel patency
Explanation: Sodium nitroprusside (Nipride) is administered after a carotid endarterectomy to decrease mean arterial pressure (MAP) and reduce the risk of hemorrhage at the surgical site. By lowering the blood pressure, it minimizes the chance of bleeding while ensuring adequate cerebral perfusion through careful monitoring. References: = AACN Handbook for CCRN Certification, pp. 75-78.
A nurse is caring for a patient who had a gastric bypass procedure 2 days ago. A physician has ordered a gastric tube to be placed due to increased abdominal distention. The nurse realizes that this procedure will most likely need to be done
A. under fluoroscopy.
B. by two nurses.
C. using ultrasound
D. with a guide wire
Explanation: After gastric bypass surgery, the altered anatomy of the gastrointestinal tract makes it challenging to place a gastric tube. Performing the procedure under fluoroscopy provides real-time imaging guidance, ensuring correct placement and reducing the risk of complications, such as perforation or misplacement.References: = CCRN Exam Handbook, page 45
| Page 2 out of 13 Pages |
| Previous |